- Home
- Brain complications
- Brain Death
Brain Death in the ICU
Unfortunately, brain death can occur in ICU patients. End of life care is as important to the ICU team as any other care or treatment provided to your loved one.

End of Life Care - Brain Death
Brain death can be difficult to understand. All states and most religions recognize it br as a legal definition of death.
Basically, the brain has permanently lost all function. Your loved one is not aware of anything. He or she cannot think, feel, hear or respond to any stimuli.
It is like a permanent coma. Other organs such as the heart or kidney do continue to function.
Brain death mostly happens after one of three events. Uncontrollable brain swelling from severe brain trauma, brain bleeding or a large stroke. Any of these can cut off all blood flow to brain and cause brain death.
The brain can also die from lack of blood or oxygen. This occurs after the heart has suddenly stopped; known as a cardiac arrest.
Any delay in restarting the heart or restoring breathing prolongs the time the brain is deprived of vital oxygen and blood flow.
If this condition last long enough the brain will die. This can vary from as little as three to possibly as long as six or seven minutes. Even with CPR the brain can sometimes still die.
Brain death can be a difficult concept to accept. For all intents and purposes the patient looks alive. The blood pressure is present and the heart still beats.
It may take time for all family members to understand an accept the situation. This is particularly true with middle-aged or younger patients.
Diagnosis of Brain Death
Many times families will be told that brain death is likely and are somewhat prepared for all of this. Most states and organized religions recognize and accept brain death
The ICU doctor at this point should inform you and the other family members that there is a high likelihood of brain death. He will tell you tests will be done to make and confirm the diagnosis.
The diagnosis of brain death first requires that two board certified doctors from specific specialties examine the patient and confirm that likely he or she is brain de
Specific tests are then performed. At the time of exam, there cannot be any drugs in the patient's system that could affect the exam.
All the normal chemicals found in the blood must be within specific, acceptable ranges.
There must be no response to any stimuli during the neurologic exam. The pupils will be dilated and not respond to light. Neurologic reflexes will not be present.
When briefly taken off a ventilator, a brain dead patient will not breathe despite elevated carbon dioxide levels; which normally stimulates us to breathe.
You may hear this referred to as the apnea test. Apnea means no breathing.
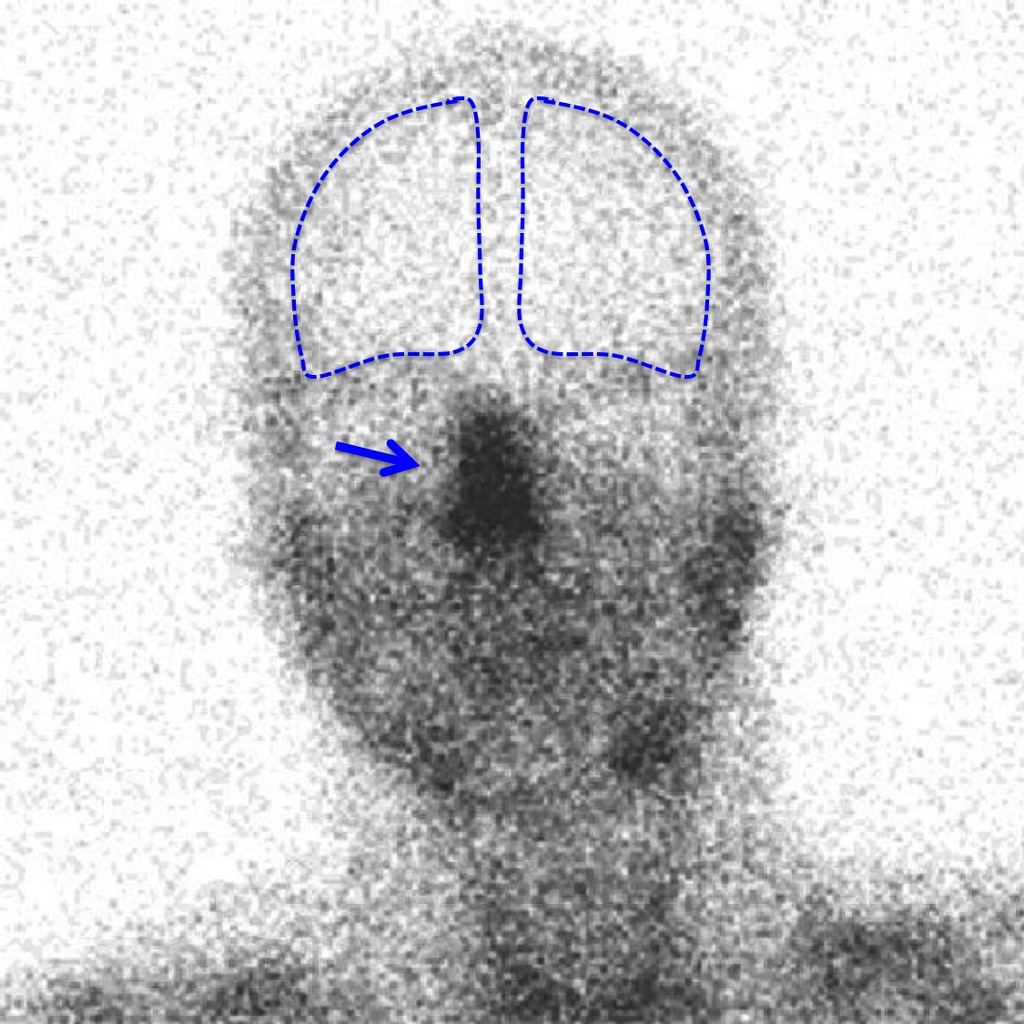
Special scans will show no blood flow to the brain.(See below)
Most hospitals do not use the EEG or electroencephalogram to determine brain death. It was never intended for this purpose.
When all these criteria are met the patient will be declared legally dead. The ICU team will inform you and your family of the results and discuss the next steps
The brain scan below shows brain death. The blue outlines the brain and inside the lines it is white. The area to the sides and top of the blue lines is the scalp. The black areas show blood flow to the nose, face and neck. There is no blood flow to the brain itself. This is brain death.
What Happens Next?
Some family members or even the entire family can have difficulty accepting brain death, As stated above, the patient still has a heart rate and blood pressure and just does not look dead.
It may take time for all this to sink in. The ICU is generally aware how difficult this time and can be. They will be there to support you and answer all your questions.
They will advise you about what to do next. You may want a member of the Clergy or other trusted friend to be with you.
After the diagnosis of brain has been confirmed and you have been told; another group in the hospital will ask you about possible organ donation.
They will explain how it works and what your options are. If you and your family decide against organ donation, it is perfectly acceptable and it will not be held against you.
If you and your family agree to organ donation, the process will be explained to you in as much detail as you desire.
In these situations it is always best if everyone in the family can agree. This may take time and private discussions with only family present. No one should feel pressured.
It can be even more difficult if some family members cannot be present because of distance, illness or other reasons. At the very least you should try to include them by phone or even ZOOM.
After all the discussions are finished, it will be time to say good by to your loved one. This might be an individual or private moment for each person. It could be everyone together.
Questions to Ask
- What if we do not accept brain death as the actual death of our loved one?
- Can we transfer our loved one to another hospital?
- Is there any penalty for refusing organ donation?
- Could we agree to donate only some organs?
- Is an autopsy necessary?
- Do we need to contact a lawyer?
- We know our loved one is brain dead and what that means; but can he or she stay in the ICU until other family members arrive?